At the annual meeting for hereditary breast and ovarian cancer in Dallas, the last thing you expect to see is Mardi gras beads.
But there they are, each color signifying something; like a cancer diagnosis or a preventative surgery. Some women wear one strand; others wear several.
Most of the women here have a mutation in the gene labeled BRCA1 or BRCA2. That means a shockingly high lifetime risk for both breast and ovarian cancer.
Cindy Salit is what’s known as a “previvor,” someone with a genetic mutation who hasn’t been diagnosed with cancer. The numbers she faces are startling; up to an 84 percent risk of breast cancer and a 62 percent risk of ovarian cancer.
“I guess my story started really with my younger sister who two years ago was diagnosed with stage II ovarian cancer," Salit says. "My OBGYN, even though my family history wasn’t that strong, suggested genetic testing and found out that I have a mutation on my BRCA2 gene.”
Salit had her ovaries removed preventatively. That was an easy choice, but there was another surgery looming.
“The decision to have my breasts removed essentially, have my breast tissue removed with a mastectomy was much harder," she says. "For me it was, well, I’ve only had one primary relative, my grandmother who had breast cancer, am I overreacting? But I knew that I was making the right decision, statistically it would be better for me to go ahead and have it done.”
Not all women with BRCA mutations catch them before cancer. Julie Shrell decided to investigate her risk after her grandmother battled breast cancer twice.
“When I turned 40 I decided I needed to go see if I was at risk and there was an assessment that I took and they came back and said that I wasn’t at risk," she says. "Fast forward eight years, I was diagnosed with ovarian cancer.”
Shrell says if she had been tested for a BRCA mutation when she first inquired about her risk, she would have had her ovaries removed then, most likely avoiding cancer.
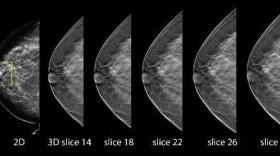
Another way to reduce risk is surveillance. Starting mammograms and MRIs early can be life saving for women who are BRCA positive. Ultrasounds and blood tests help doctors catch ovarian cancer. Maintaining a healthy body weight can have an impact as well.
The problem is a lot of people with hereditary cancer risk just don’t know it. Dr. David Euhus is the Medical Director of Clinical Cancer Genetics at UT Southwestern.
“I see women all the time whose mothers had breast cancer at 75 and they are extremely anxious about being high risk for breast cancer. And those women are not at increased risk at all, generally speaking. Then have women, oh, my aunt had ovarian cancer and grandmother had breast cancer at 48, and they don’t put any of that together.”
So what should you look for in your own family when deciding on genetic testing?
Anyone who’s had a breast cancer before the age of 45, anyone with ovarian cancer in the family, anyone with a male breast cancer, anyone with triple negative breast cancer, that’s a sub type of breast cancer before the age of 60.
If that doesn’t sound like you, you’re not off the hook. Here’s Dr. Rick Boland, Director of the GI Cancer Research Lab at Baylor.
“Lynch Syndrome is a hereditary disease that predisposes people to early onset cancers of the colon, of the uterus and a few other places too.”
Boland says Lynch Syndrome is more prevalent than a BRCA mutation, and probably less understood.
“It’s probably the commonest hereditary form of cancer in the population, probably 1 in 350 or something like that has it. The problem is that since the people look perfectly normal and there’s not anything you can measure short of finding the genetic abnormality, most people who have it, don’t know that they have it," he says.
He recommends genetic testing for early onset cancers of the colon, uterus, ovaries and stomach.
And those who test positive for Lynch syndrome require a battery of annual screenings like colonoscopy and endometrial biopsy.
Another option is preventative surgery to remove the uterus and ovaries.
“Unlike some very unfortunate disease, let’s say, Huntington’s chorea, or something like that, if you have that mutation there’s really nothing you can do to stop the devastating medical consequences," Boland says. "But with Lynch Syndrome, you can avoid most of the problems with appropriate surveillance.”
Euhus says people with family risk should see a genetic counselor.
“I still run into patients very frequently who say, what’s the sense of doing genetic testing, all it is going to do is give you bad news and there’s nothing you can do about it," he says. "That is just so far from the truth.”
Just ask ovarian cancer survivor Julie Shrell.
“Actually, it is very empowering, because you’re not standing there going, ok, it’s going to hit me and there’s nothing I can do about it," she says.
And she hopes others will tap into that power too.
Courtney Collins was recently diagnosed with Lynch Syndrome. She shares how the news changed her lifestyle, and what it's like to be screened for genetic cancers.